The Affordable Care Act (ACA), enacted in March 2010, was created with the goal to make healthcare more affordable. All applicable large employers (ALEs) with 50 or more full time, or full time equivalent employees must offer ACA compliant benefits to at least 95% of their workforce, and their dependents.
ALEs who do not comply with this federal requirement are subject to heavy fines and penalties from the Internal Revenue Service (IRS).
Each year, the IRS requires ALEs send their employers 1094 and 1095 documents to fill out to make sure their employers are complying with ACA requirements. It also helps the IRS ensure ALEs are offering coverage, and the type of coverage offered. Let’s dive into what forms 1094 and 1095 are. Each employee must fill out their healthcare information and submit it back to the IRS.
What is ACA Form 1094?
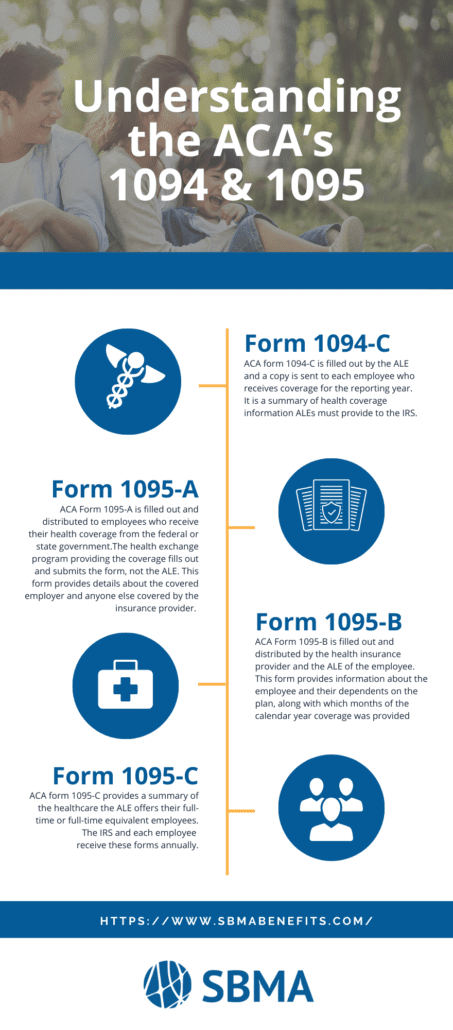
ACA form 1094-C is filled out by the ALE, and a copy is sent to each employee who receives coverage for the reporting year. It includes information such as:
- Contact information
- Certifications of Eligibility
- The Aggregated ALE group Members
- The ALE’s address, number, EIN
- Number of full-time or full-time equivalent employees and the total number of employees
Form 1094-C is a summary of health coverage information ALEs must provide to the IRS
What is ACA 1095?
The form provides a summary of the healthcare information the ALE offers their employees along with the ALE’s information.
There are three different types of Form 1095:
- Form 1095-A
- Form 1095-B
- Form 1095-C
ACA Form 1095-A is filled out and distributed to employees who receive their health coverage from the federal or state government such as Medicare, Medicaid, or TRICARE. The government health exchange program providing the coverage for form 1095-A fills out and submits the 1094-A form, not the ALE. This form provides details about the covered employer and anyone else covered by the insurance provider.
ACA Form 1095-B is filled out and distributed by the health insurance provider and the ALE of the employee. This form provides information about the employee and their dependents on the plan, along with which months of the calendar year coverage was provided. Information on the form includes:
- Name of the employee
- Date of birth
- ALE information
ACA form 1095-C provides a summary of the healthcare the ALE offers their full-time or full-time equivalent employees. The IRS and each employee receive these forms annually. The form includes information such as:
- Healthcare coverage offered and if it meets ACA requirements
- What months the coverage was available to the employee
- The lowest cost premium provided
- Employee contribution amount
- Employee enrollment dates
This form must be submitted to employees by January 31st and to the IRS on March 31st. Filing can be completed online or by paper. However, paper submissions are due earlier, by February 28th. Keep in mind that file forms 1094-C and any 1095-C form must be filed together.
According to the IRS, “Form 1094-C is used to report to the IRS summary information for each employer and to transmit Forms 1095-C to the IRS. Form 1095-C is used to report information about each employee.” Both forms are important because the information they report helps the government agency determine if the ALE is liable for payment, and if they are compliant with federal regulations.
How can SBMA help you?
SBMA offers affordable ACA-compliant Minimum Essential Coverage benefits for employers. For more information on MEC and what it covers, read our article here.