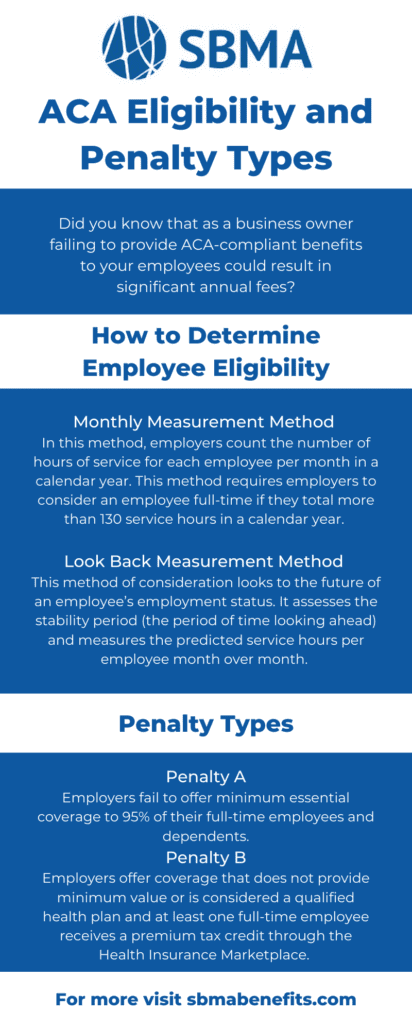
There are two different penalty charges that businesses are responsible for in the event that they fail to provide adequate health coverage for eligible employees.
Penalty A
Penalty A will come into effect when employers fail to offer minimum essential coverage to 95% of their full-time employees and dependents. In order to avoid this penalty, you must determine who is considered a full-time employee, or full-time equivalent employee, and should be receiving benefits.
Penalty B
Penalty B occurs when employers that offer coverage to their full-time employees, offer coverage that does not provide minimum value or is considered a qualified health plan and at least one full-time employee receives a premium tax credit through the Health Insurance Marketplace.
We’ve made it simple to calculate the costs you can expect to be responsible for in fines and penalties should you fail to provide required coverage for eligible employees. Utilize our calculator below to estimate the associated costs based on the estimated number of full-time eligible employees that you have.
Minimum Essential Coverage (MEC) benefits are exactly what it sounds like. They are the minimum coverage to meet ACA requirements for eligible employees. Offering MEC benefits is an affordable and compliant way to provide coverage to all eligible employees and avoid ACA regulatory fees and penalties. This tool takes things one step further by comparing potential ACA penalties with the cost of providing MEC benefits to eligible employees.
Check out one of our latest blog posts for more information and details on the MEC plans offered by SBMA Benefits.
For more information about employer mandate penalties for 2023 and 2024, check out our guide, here.