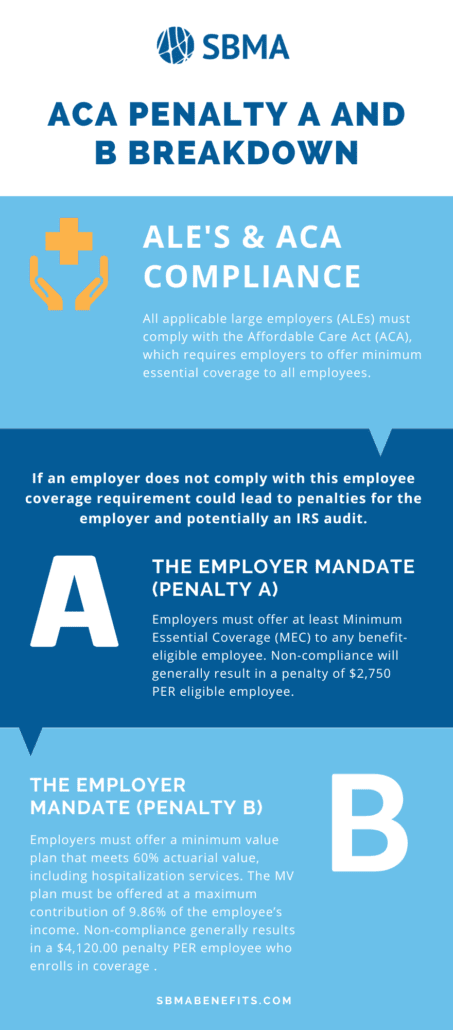
ACA Penalty A and B Breakdown
All applicable large employers (ALEs) must comply with the Affordable Care Act (ACA), which requires employers to offer minimum essential coverage to all employees.
If an employer does not comply with this employee coverage requirement, it could lead to penalties for the employer and potentially an IRS audit.
Below is a breakdown of ACA penalties A and B and how they could affect your company.
Who is Considered a Large Employer?
First, who is considered a large employer?
Any company or organization with an average of at least 50 full-time employees or “full-time equivalents (FTEs) is considered an applicable large employer.
*For the purposes of the ACA, a full-time employee is someone who works a minimum of 30 hours a week.
What Are ACA Benefits?
The ACA was created in 2010 to offer more affordable health benefits to a wider range of people. Any ACA-compliant benefit plan must cover these 10 health benefits:
- “Ambulatory services
- Emergency services
- Hospitalization
- Pregnancy, maternity, and newborn care (before and after birth)
- Mental health and substance use disorder services
- Prescription drugs
- Rehabilitative and habilitative services and devices
- Laboratory services
- Preventative and wellness services and chronic disease management
- Pediatric services”
Additionally, ACA benefits cover birth control and breastfeeding support.
The Employer Mandate (Penalty A)
Employers must offer at least Minimum Essential Coverage (MEC) to any benefit-eligible employee. Non-compliance will generally result in a penalty of $2,750 annually PER eligible employee.
The Employer Mandate (Penalty B)
Employers must offer a minimum value plan that meets 60% actuarial value, including hospitalization services.
The MV plan must be offered at a maximum contribution of 9.86% of the employee’s income – YOU pay the difference.
For example, take a California minimum wage employee: A $10.00/hour employee working a minimum of 30 hours per week has a maximum employee contribution of $128.18 per month.
If the plan cost is $300, YOU pay the difference of $171.82 per month.
Non-compliance will generally result in an annual $4,120.00 penalty PER employee who enrolls in coverage through the state exchange AND receives a premium subsidy.
The Individual Mandate
The individual mandate went away starting January 1st, 2019, for most Americans.
Those individuals in specific states that maintain the individual mandate, including the District of Columbia, Massachusetts, or New Jersey, will continue to be penalized according to the individual mandate.
These penalties can easily add up with over 100 employees eligible for health coverage. At SBMA, we want to help you avoid any potential penalties for lack of proper insurance.
Contact an SBMA representative for more information regarding your employer benefit needs.