Who Now Covers Surprise Medical Costs?
Before the No Surprises Act, the insured individual was liable for any “surprise costs” that arose after receiving emergency services. With the new regulations, any surprise billing that arises is the responsibility of the medical establishment providing the care and insurance provider to negotiate payment. Fees for surprise billing will be based on the No Surprises Act’s new term called the Qualifying Payment Amount (QPA).
What is the QPA?
The QPA finds the median rate for plans in the surrounding location for in-network services.
Institution and Insurer can negotiate to settle on a fair payment, or they can turn to an Independent Dispute Resolution (IDR) entity to decide a fair payment amount. To find fees due, the IDR will collect what the provider and the plan deem fair payment amounts for the out-of-network service. After offers are submitted, the IDR will factor variables such as QPA, market shares, patient information, provider level of expertise, and more to reach a fair decision.
According to KFF, “the IDR will charge a fee for each arbitration and the losing party must pay that fee.” Fees can range from $200-$600 depending on the case.
Can Providers ask Consumers to Waive Rights?
There is one exception to the No Surprises Act, and that is for providers to ask patients to waive their rights under the No Surprises Act. It is allowed if patients give prior written consent and agree to be billed more by out-of-network providers. However, there are exclusions to what providers can ask plan holders to waive rights to.
Consent waivers are not allowed for the following services:
- Emergency services
- Unforeseen urgent medical needs during non-emergent care
- Ancillary services
- Services provided by a hospitalist, or assistant surgeon
- Out of network provider services if there is not an in-network provider available
- Diagnostic service
Plan holders must give consent voluntarily and cannot be persuaded to waive their rights.
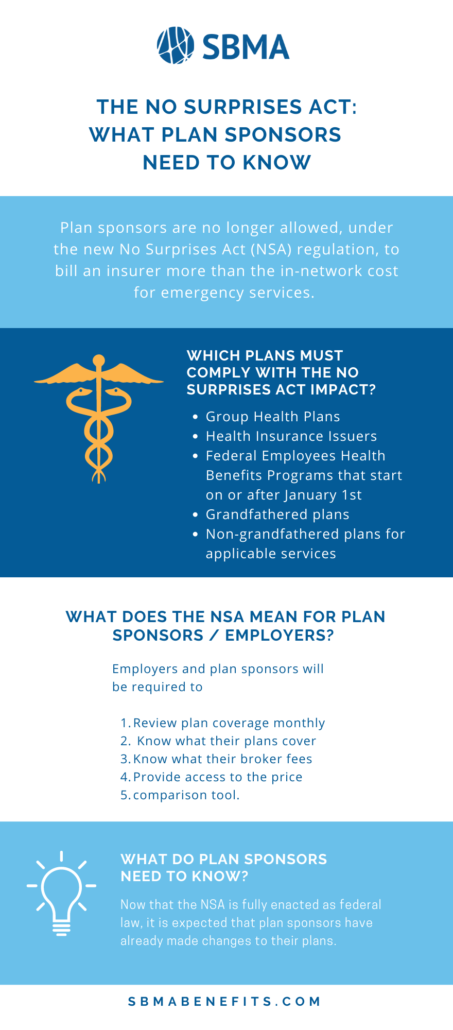
For more information read our article about everything you need to know about the No Surprises Act.