Over the past two years, employees have been leaving their jobs in record numbers. In fact, this phenomenon, termed The Great Resignation, resulted in 20 million people leaving their jobs in the second half of 2021 alone. Due to mass resignations, employers are searching for solutions to successfully recruit and retain employees.
There are, of course, a variety of factors that contribute to an employee’s decision to leave or stay with a company. Today, we’ll be discussing just one of these factors: How health benefits can contribute to employee recruitment and retention.
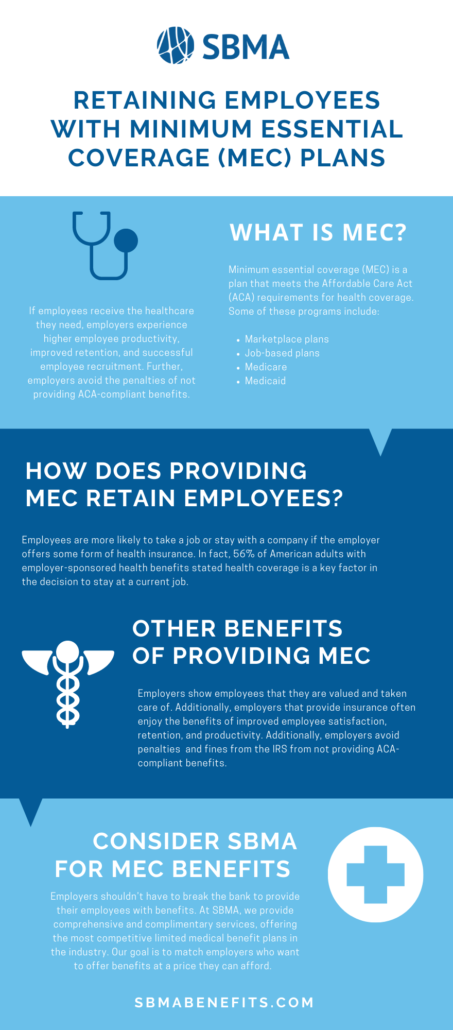
If employees receive the healthcare they need, employers experience the results of higher employee productivity, improved retention, and successful employee recruitment. Further, employers avoid penalties for not providing benefits complying with ACA requirements.
Let’s start with breaking down what MEC is and what these plans cover.
What are Minimum Essential Coverage Benefits?
Minimum essential coverage (MEC) is a plan that meets the Affordable Care Act (ACA) requirements for health coverage. Some of these programs include:
- Marketplace plans
- Job-based plans
- Medicare
- Medicaid
*All applicable large employers (ALEs) with 50 or more full-time or full-time equivalent employees are required by law to provide ACA-compliant health coverage to their employees. ALEs who do not provide ACA-compliant coverage are subject to fines and penalties from the Internal Revenue Service.
Read on for more information about MEC.
How Does Providing Minimum Essential Coverage Recruit and Retain Employees?
The bottom line is that employees are more likely to take a job or stay with a company if the employer offers some form of health insurance. In fact, 56% of American adults with employer-sponsored health benefits stated that health coverage is a key factor in their decision to stay at a current job.
How Can Employers Retain Employees with Minimum Essential Coverage?
By providing MEC, employers show employees that they are valued and taken care of. Additionally, employers that provide insurance often enjoy the benefits of improved employee satisfaction, retention, and productivity.
What Minimum Essential Coverage (MEC) Options Are Available?
There are three different plan options available. Employers should be familiar with the differences between levels of coverage so they can best decide which MEC plan works for their employees. The levels of coverage include:
Standard Minimum Essential Coverage Plans
Standard MEC plans are ACA compliant and include coverage for wellness, preventative services, prescription discounts, and telehealth services.
Enhanced Minimum Essential Coverage Plans
Enhanced MEC plans take coverage one step further than standard plans. These plans are aimed at attracting and retaining top talent by also including primary and urgent care visits with low copays and discounted specialist and laboratory services.
The Highest-Level Minimum Essential Coverage Plans
The highest-level MEC plans include the enhanced MEC plan benefits along with added coverage such as prescription coverage and low copays.