When seeking out health insurance coverage past when it’s partially covered by your previous employer, how do you choose between picking COBRA or private health insurance?
Both have pros and cons. The right choice, however, depends on your unique circumstances.
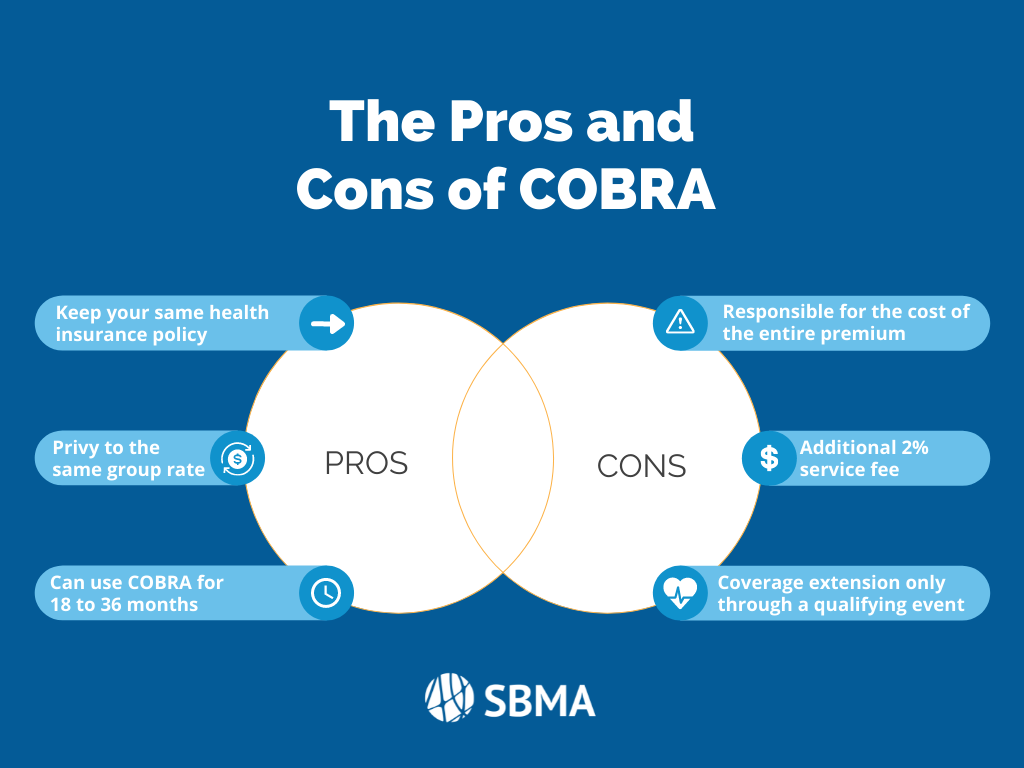
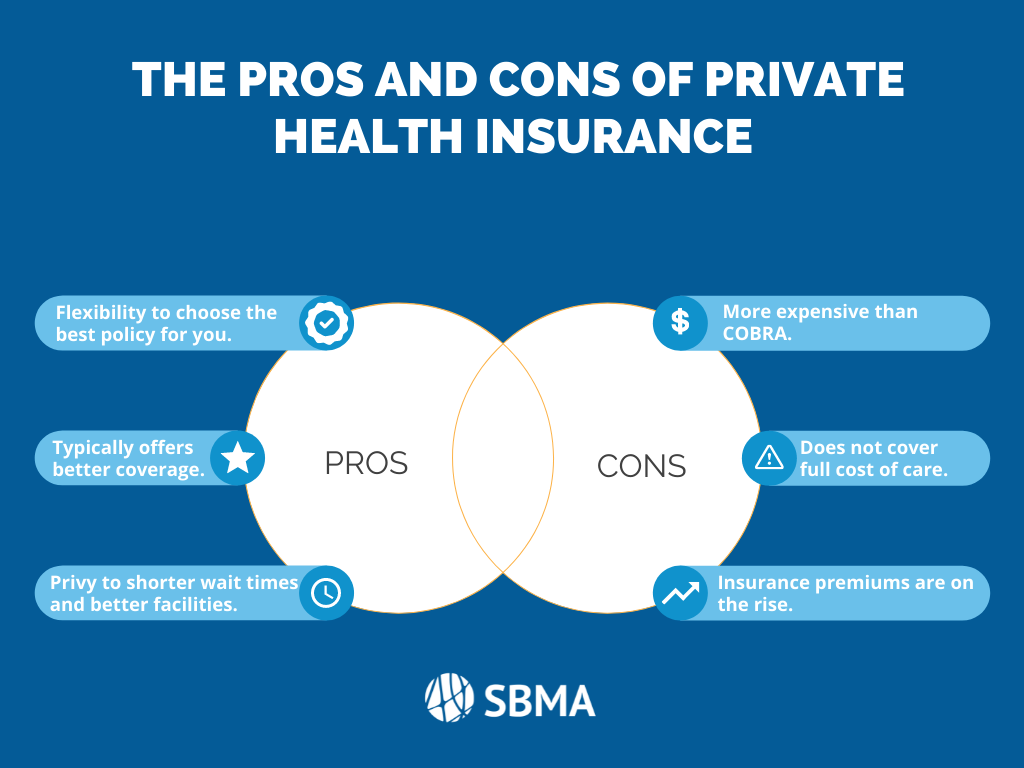
Let’s discuss the pros and cons of COBRA vs. private health insurance.
What is COBRA?
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is not insurance itself. Alternatively, COBRA is a law that was passed in 1985.
This law, COBRA, allows employees to continue on their existing health insurance plan if:
- They are reduced to work less than 30 hours a week, or
- Leave their job voluntarily or involuntarily
Under COBRA, the employee continues on his or her insurance plan but is then responsible to cover the entire cost. It is no longer the employer’s responsibility to cover health insurance premiums as they had previously.
COBRA, however, is not available to everyone. COBRA is only available to employees who worked at a public or private company with 20 or more employees.
What is Private Health Insurance?
Private health insurance, on the other hand, is any health insurance policy plan that is not run by a government-run insurance plan (i.e. Medicare, Medicaid, Obamacare).
This type of coverage, though not government-run, must comply with state and federal insurance regulations.
Depending on the type of insurance policy, regulations include:
- Affordable Care Act (ACA) essential health benefits
- Maternity care
- Meeting minimum essential coverage (MEC) requirements
- Providing minimum value to avoid employer mandate penalty
- Capping in-network and out-of-pocket costs