What is the Build Back Better Bill?
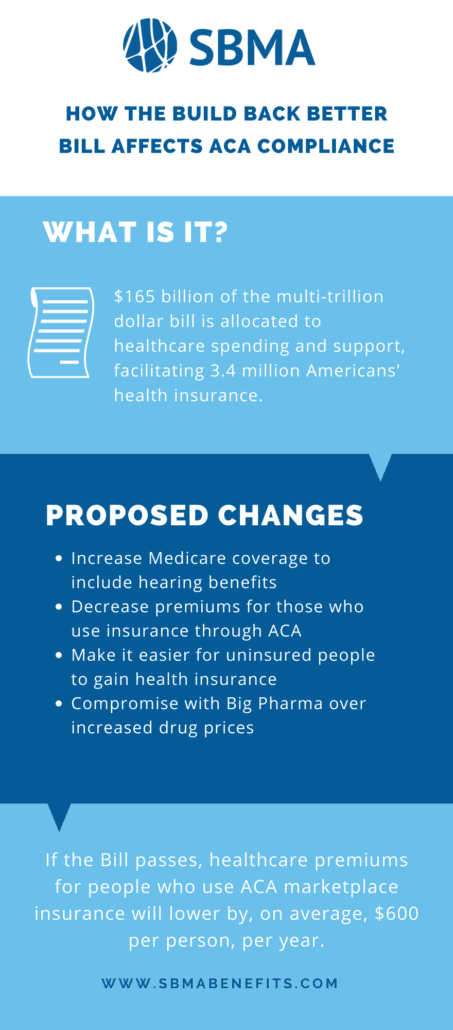
The Build Back Better framework, created by the current administration, is engineered to “set the United States on course to meet its climate goals, create millions of good-paying jobs, enable more Americans to join and remain in the labor force, and grow our economy from the bottom up and the middle out”. One of the elements of the bill allocates $165 billion to healthcare spending and support. $35 billion is earmarked for adding hearing services to existing Medicare coverage with $130 billion earmarked for Affordable Care Act (ACA) credits, including coverage for previously uncovered states.
The New York Times estimates that the Build Back Better Bill will facilitate the coverage of 3.4 million Americans who do not currently have health insurance. The Build Back Better Act aims to expand healthcare access for children, and make health insurance more affordable for the general population. The Biden administration’s goal is to close the gap in insurance coverage and move America toward universal health coverage.
According to the White House briefing room statements regarding the Build Back Better Bill, “the Build Back Better framework will expand access to affordable coverage. In all, the framework will be the largest expansion of health care coverage since the Affordable Care Act.”
The Proposed Changes and What They Could Mean
The proposed changes through the Build Back Better Bill include:
- Increased Medicare coverage to include hearing benefits
- Decreased premiums for those who use insurance through the ACA
- Streamlined processes for uninsured people to gain health insurance
- Negotiations with Big Pharma over drug prices
If the Bill passes, healthcare premiums for people who use ACA marketplace insurance will lower by, on average, $600 per person, per year. This will impact over 9 million Americans and is predicted to help insure over 3 million people who would otherwise remain uninsured. In an example given by the White House, “a family of four earning $80,000 per year would save nearly $3,000 per year (or $246 per month) on health insurance premiums.”
Additionally, the bill would provide ACA premium tax credits to up to 4 million uninsured people who live in states where they are locked out of Medicaid. The framework of the Bill sets premiums for these specific individuals at $0 to enable access to affordable and accessible healthcare.
Finally, the framework restricts drugmakers as to how much they can increase drug prices annually and limits out-of-pocket spending on drugs that have been on the market for over 10 years. Possible repercussions of the 10-year cutoff might be an increase in costs for newer drugs with drugs nine years or older then becoming more affordably priced.
One of the proposed changes for drug-making companies is to cap the prices of insulin for diabetes treatment at $35 for a 30 day supply. Currently, insulin can cost as much as $300 per vial. Another part of the drug pricing legislative proposal would cap prescription drug spending on an annual basis.
Learn more about ACA deadlines and compliance requirements in our guide, here.