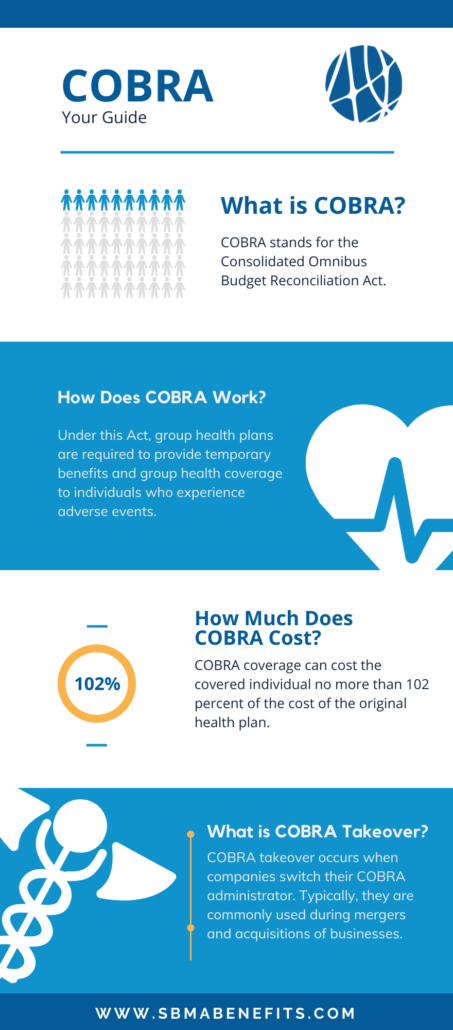
How Much Does COBRA Cost?
COBRA coverage can cost the covered individual no more than 102 percent of the cost of the original health plan. According to the U.S. Department of Labor, “In determining COBRA premiums, the plan can include the costs paid by employees and the employer, plus an additional 2 percent for administrative costs.”
The premium can cost on average $400-$700 a month per person. In order to calculate the cost of COBRA continuation coverage, add how much the employer contributes to the health plan, plus how much the employee contributes to the health plan, then multiply the sum by 2% for the service fee. Please see the formula below:
(Employer contribution to coverage + Your Contribution) x 0.02% = COBRA Premium)
For example, an employer who contributes $400 a month for an employee who contributes $200 a month would bring the total to $600 towards contributions. Multiplied by the 2% charge, the COBRA cost each month would cost $612 each month.
What is COBRA Takeover?
COBRA takeover occurs when companies switch their COBRA administrator. Typically, they are commonly used during mergers and acquisitions of businesses. Employers thinking about M&A plans should consider taking the advice of an attorney to include the right COBRA language in the M&A contract.
If one company acquires another, then the first company, let’s name it company A, can decide to take the responsibility of COBRA coverage for employees instead of the second company, company B. However, if company A sells their business or becomes bankrupt, then becomes bankrupt, company B would then be responsible for employee COBRA benefits.
How to Apply for COBRA Takeover?
Each health plan has a different procedure for applying for COBRA benefits and processing claims. Best practice is to contact your plan administrator. To download a COBRA Takeover application, and learn more about COBRA, click the link here.